Biography
Interests
Ana Lazarova
University Clinic for Surgery Disease St.Naum Ohridski Skopje, R. Macedonia
*Correspondence to: Dr. Ana Lazarova, University Clinic for Surgery Disease St.Naum Ohridski Skopje, R. Macedonia.
Copyright © 2021 Dr. Ana Lazarova. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Orbital mucoceles are cysts which are filled with mucous fluid that cannot naturally drain from the
nose. Most common arising from the ethmoid or frontal sinuses they grow and slowly cause mass
effect of the adjacent orbital tissues.
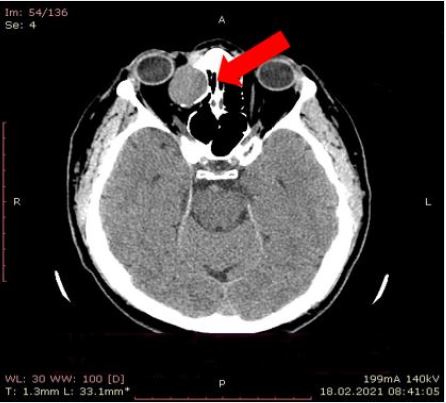
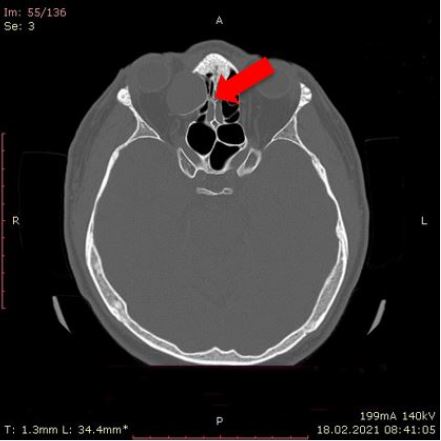
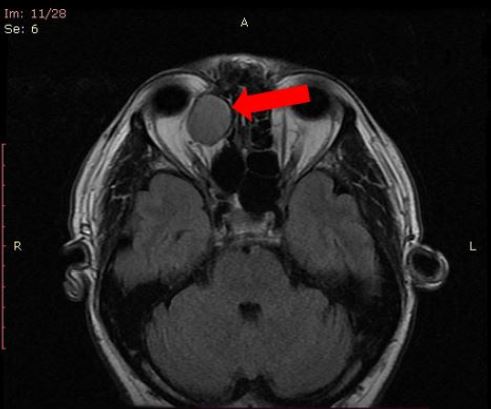
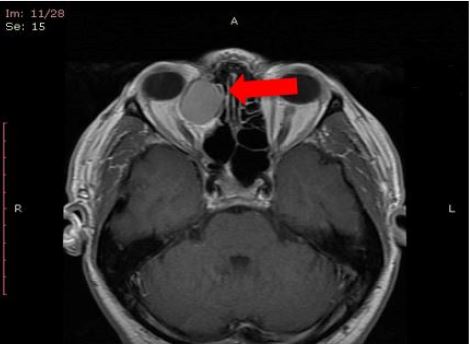
This is a case of 46 years old patient who present with symptoms of exophthalmos and pain in
the right eye, in a period of one year. After ophthalmology examination he was send for magnetic
resonance imaging (MRI) of the orbital cavity to be done. MRI was done in standard T1 and T2
waited images and waited images after contrast administration. In the right orbital cavity lokalizated
in the extraconal space adherent to the ethmoidal cellules, oval homogenous tumor formation with
the diameter of 26mm was found. This formation was with intermediate signal intensity in T1
waited images and low signal intensity in T2 waited images which suggested that is present like
a solid tissue, because is protein -rich content. In the waited images after contrast administration
there was periphery contrast enhancement. There was no invasion of the optic nerve or other conal
eye structures, but there was mass effect of the medial rectus muscle with the displacement of all conal structures laterally. The lateral wall of ethmoidal cellules was disrupted and part of them
next to the tumor were displaced Also computer tomography (CT) scan was preformed, for better
evaluation of the sinus structures as additional investigation. The density of solid tissue was confirmed
and no calcification in it was found. Neurosurgery with Misonix ultrasonic knife was performed
and encapsulated dense cystic formation was found and send to pathohistology verification with
the result for mucocele.
This is an interesting case of atypical presentation of sinus mucocele which can mimic benign
orbital cavity tumor mass and MRI diagnosis of mucocele in orbital cavity should be considered
especially when communication with nearby sinus can be predicted on the images. Although those
are benign lesions, still their expansive behavior may cause paranasal sinuses bone erosion and with
compression might compromise the adjacent structures. Early diagnosis is essentially for adequate
treatment.
Introduction
Orbital mucoceles are cysts which are filled with mucous fluid that cannot naturally drain from the nose.
Most common arising from the ethmoid or frontal sinuses they grow and slowly cause mass effect of the
adjacent orbital tissues [1,2].
Mucocele of a paranasal sinus is consisted of mucous secretion that accumulates trough time together with desquamated epithelium within the sinus which results in distension of its walls. It presentation is as a cyst like lesion but often the mucocele has expansive and destructive behavior [3,4].
The frontal sinus with occurrence of mucoceles there in 60-89%, is the most common side whereas sphenoid, ethmoid, and maxillary mucocoeles are rare. There is no difference between the affection of male and female population. Sometimes presence of infection might be found in the culture of the aspirated mucocele [5].
Mucocoeles sometimes might behave like tumor formation that cause bone erosion and the displacement of nearby structures. The most common sites of extension are orbital cavity or intracranial extension. As a result of erosion of the posterior wall of the frontal sinus intracranial extension occurs and complication of it might lead to meningeal inflammation or cerebrospinal fluid fistula. The posterior sinus wall has predisposition to erosion because of its thickness. In case of presence of infection there is a higher tendency for bone erosion [6].
The etiology of mucoceles is different and multifactorial but inflammation is the leading factor for mucoceles occurrence. The important thing that makes mucoceles look hazard is the fact that sinuses are nearby the orbit and brain so mucoceles might spread in to the orbital cavity or intracranially [7].
Firstly diagnosis of mucocele is based on clinical investigation and then radiology investigation methods come in matter basically computed tomography (CT) and then magnetic resonance (MR) imaging [8].
CT is used in determining the size of the lesion, regional anatomy position and extent of the lesion, specifically if its aggressive behavior comes in matter and the bony erosion is present with its displacement in orbital cavity or intracranial. MR imaging is useful in establishing the definite diagnoses of mucoceles, differencing from neoplasms especially via contrast enhancement [9].
The main treatment of mucoceles is surgery, which differs from endoscopic sinus surgery than craniotomy, and craniofacial exposure, with or without obliteration of the sinus. Better understanding the pathophysiology of mucoceles also influence of improving the surgical treatment which result into less invasive procedure which emphasize more on surgical drainage over ablation [10,11].
Case Report
This is a rear presentation of mucocele localized in medial part of orbital cavity mimic neoplasm.
This is a case of 46 years old patient who present with symptoms of exophthalmos and pain in the right eye, in a period of one year. After ophthalmology examination he was send for magnetic resonance imaging (MRI) of the orbital cavity to be done. MRI was done in standard T1 and T2 waited images and waited images after contrast administration. In the right orbital cavity localized in the extraconal space adherent to the ethmoidal cellules, oval homogenous tumor formation with the diameter of 26mm was found. This formation was with intermediate signal intensity in T1 waited images and low signal intensity in T2 waited images which suggested that is present like a solid tissue, because is protein -rich content. In the waited images after contrast administration there was periphery contrast enhancement. There was no invasion of the optic nerve or other conal eye structures, but there was mass effect of the medial rectus muscle with the displacement of all conal structures laterally. The lateral wall of ethmoidal cellules was disrupted and part of them next to the tumor were displaced Also computer tomography (CT) scan was preformed, for better evaluation of the sinus structures as additional investigation. The density of solid tissue was confirmed and no calcification in it was found. Neurosurgery with Misonix ultrasonic knife was performed and encapsulated dens cystic formation was found and send to pathohistology verification with the result for mucocele.

Discussion
The mucoceles are not malign lesions, grow slowly with predisposition of occurrence in frontal or ethmoidal
group of sinuses, pressure of growing may lead to erosion of the adjacent bone structures. The sac may be
filled with pus as a result of chronic infection, which is known as a chronic mucopyocoele [12,13].
Stimulation of lymphocytes and monocytes which leads to the production of cytokines by the lining fibroblasts occurs as a result of frontal recess obstruction and repetitive infections. These cytokines by time promote bone resorption and remodeling that result with in expansion of the mucocele. Significantly elevated levels of prostaglandin E2 and collagenase are produced by the fibroblasts derived from frontal and ethmoidal mucoceles, in comparison with normal frontal sinus mucosa fibroblasts where those levels are lower. High levels of prostaglandin E2 has a important role in the osteolytic process in mucocoeles which is one explanation for their local aggressive behavior [14,15].
Clinical symptomatology of mucocoeles is slightly different in correlation with it’s the localization.
In the position when mucocoela migrates in orbital cavity it behaves as a tumor and ophthalmological manifestations occur, such as impaired visual acuity, reduced ocular mobility, diplopia and exophthalmos [16,17].
Radiologic findings are the bases of establishing the diagnosis together with the physical examination and good anamnestic data. Based on CT scan diagnosis of a mucocoele might be consider if there is finding of oval or round homogeneous dense mass with clearly defined margins. If the mucocele has high protein content or hemorrhage it present with intermediate to high signal intensity on T1 waited images which may lead to misdiagnosis [8,13].
Differential diagnosis that comes in matter especially when mucoceles migrate in orbital cavity or intracranial are: dermoid cysts, histiocytosis, fungal and tuberculosis infections, orbital cholesterol granuloma, and other uncommon neoplasms [18].
Conclusion
This is an interesting case of atypical presentation of sinus mucocele which can mimic benign orbital
cavity tumor mass and MRI diagnosis of mucocele in orbital cavity should be considered especially when
communication with nearby sinus can be predicted on the images. Although those are benign lesions, still
their expansive behavior may cause paranasal sinuses bone erosion and with compression might compromise
the adjacent structures. Early diagnosis is essentially for adequate treatment.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!