Biography
Interests
Morteza Alibakhshikenari
Department of Medical Sciences and Health Services, University of Sari, Iran
*Correspondence to: Dr. Morteza Alibakhshikenari, Department of Medical Sciences and Health Services, University of Sari, Iran.
Copyright © 2020 Dr. Morteza Alibakhshikenari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Health and wellbeing of employees in the workplace are important concerns that should continue to receive attention in any organisation. Traditionally hospitals are directed towards curative services, not preventive services, it is very important to maintain optimum health of the staff in the healthcare industry as they take care of the sick clients. The study was conducted with the major objective to assess the risk and hazards faced by nurses in different clinical areas of work (Units). Quantitative descriptive cross-sectional method was used for the study. The study was conducted with a sample of 588 respondents (unit managers, registered nurses and assistant nurses). The findings revealed that nurses do encounter a considerable level of occupational hazards. Critical Care and Cardiology Unit were found to be the units with the highest risk of occupational hazards and injuries while the lowest risk was observed in the outpatient and day care unit. Chi square analysis of data revealed a significant association of Clinical Area of work (Unit) with exposure to blood borne pathogens & biological hazards, radiation, toxic fumes & anaesthetic agents, irritation from disinfectants & sterilants and chemical/toxic medication.
Introduction
Healthcare professionals form a huge global work sector, and are crucial for the healthy sustenance of people
of any nation. The most constant injuries reported among healthcare professionals are musculoskeletal
disorders, burns and fractures and the most commonly occurring illnesses are upper respiratory tract
infections, skin and hepatic disorders and drug reactions. There are many identified chemicals used in the
hospitals that have adverse effects on people working in the environment.
According to Bureau of Labour Statistics (2015), the most common nature of non-fatal injury or illnesses reported among nurses were sprain, strain, and tears. Many of these illnesses were serious resulting 31 or more days away from work. It is necessary to identify and reduce the exposure to risks in their working environment as these risks not only influence their own health but also affect patient care. In the nursing workplace environment, many stressors are present that can lead to diseases and injuries, these hazards can impair the health status acutely or in long term. The awareness of occupational hazards is minimum among the nurses [1]. As per the Bureau of Labor Statistics (2012) nurses are sustaining occupational injuries, particularly work-related musculoskeletal injuries and disorders almost twice the national rate of the general population due to their work. Most of the studies on occupational health have focused mainly on worker’s compensation, insurance, absenteeism, and economic consequences towards the organisation. Very little focus is made towards the impact on the life of the workers affected due to workplace injuries and illnesses. The repercussions of these workplace injuries reach the victim’s workplace, home, hospitals, courts, and the local community. The type and severity of the illnesses or injuries matter a lot to define its consequences and effects for e.g. an employee with a severe disabling back injury will face more consequences than an employee with minor sprain will.
The study was conducted with the major objective to assess the risk and hazards faced by the nurses in different clinical areas of work (Units).
Literature Review
The healthcare providers are rated third among major groups besides Labourers/freight workers and truck drivers who experience a high number of workplace injuries mainly because of direct patient care (Bureau of Labor Statistics, 2012). In a study on the effect of transfer, lifting and repositioning procedures among health care providers out of the total injuries among the health care providers, nurses were found to be the most affected, mainly with back, neck and shoulder injury [2]. Holman et al. (2010) [3] reported that in a shift, 20% of the time spent by nurses is on patient handling task and the job culture of nurses during patient handling situations is always to consider patient safety above their own. 40% of nurses believed that sprain, strain and a sore back is the part of their job. Approximately 20% of nursing jobs include patient handling and mobilisation; that is the reason adequate training on safe patient handling and mobilisation is essential. In a study conducted by Zaidi et al. (2012) [4] most of the health care providers preferred to treat themselves rather than opting to follow hospital protocol and incident reporting system. Shreedharan et al. (2011) [5] reported that 97% of nurses were familiar with the idea of standard precautions. 61.2% believed that all patients’ blood and body fluids are potentially infected whereas 27.6% thought only diagnosed patients are infected and 11.2% believed only patients who are suspected of infection are infectious. The study emphasised to implement an educational program to improve the knowledge of nurses on standard precautions. Collins (2010) [6] reported that health care workers are more prone to musculoskeletal disorders when compared with other jobs, which are physically more demanding like in construction, mining, and manufacturing. The main reason for musculoskeletal injuries in health care workers is due to positioning, transportation and assisting patients. (Schoenfisch et al., 2013) [7]. Among all occupations, nursing is ranked highest for musculoskeletal disorders ranging from 40-80% among all populations [8]. Dawson (2012) [9] reported that 62% of nurses had reported disabling musculoskeletal injury was their major concern and 56% had experienced musculoskeletal pain, which was worsened due to the nature of their job.
The main reasons for leg and foot pain symptoms in nurses working in intensive care units are due to shift duties and longer working practice [10]. Prolonged untreated MSDs that is symptoms more than 6 months of the period can lead to sickness, absenteeism and significantly decreased productivity (Taylor and Green, 2015). Working condition of nurses includes several risk factors, for example, operation theatre nurses experience prolonged twisted and static postures [11], Roll, et al. (2012) [12].
Approximately £600,000 per year is the estimated cost towards needlestick injuries that is compensated by NHS in the United Kingdom, including prophylaxis treatment, lab investigations, treatment, counselling and legal procedures [13]. Many articles have reported that one of the reasons for needle stick injuries is a feeling of urgency. In a study of 33,327 Taiwanese nurses on work-related injuries and illnesses done by Chiou et al. (2013) [14], the findings revealed that the nurses working in critical care areas and operating rooms have highest levels of radiation exposures. Health care workers are more at risk for infections as they are in close contact with patients and handle human biological wastes like sputum, faeces, urine, blood and this can also lead to public health implications as health care workers can be a source of transmission to other patients and other people in the community associated with them [15]. Importance of respiratory protectors for direct patient caregivers should be emphasised. In 1.3 million workplaces, around 5 million U.S workers were asked to wear respiratory protection to minimise inhalation exposures (OSHA, 2016).
It is very important to explore factors that contribute to work-related injuries and illnesses for maintaining a healthy and safe work environment to enhance healthcare professional’s health and promote quality patient care.
Materials & Methods
Quantitative descriptive cross-sectional method was used for the study by using a wide range of Demographical variables (age, work experience, professional experience, training, the risk associated with work etc). The study was carried out in a multi speciality 600 bedded hospital catering the needs of both nationals and multinationals being admitted in the hospital, in order to assess the association (if any) of risk factors with the clinical ares of work (Units).
The convenience sampling method was used for the study. The study was carried out among nurses (Unit
Managers, Registered Nurses and Assistant Nurses) who were involved in direct or indirect patient care. The
data was collected using
A sample of 68 nurses was obtained using purposive sampling technique. The pilot study participants varied in diversity to ensure proper representation of the available population.
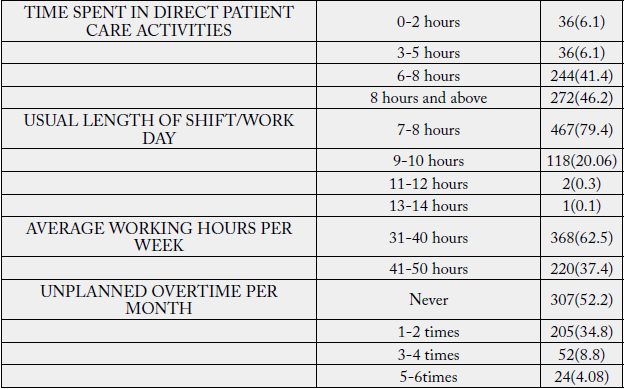
Findings of the Study
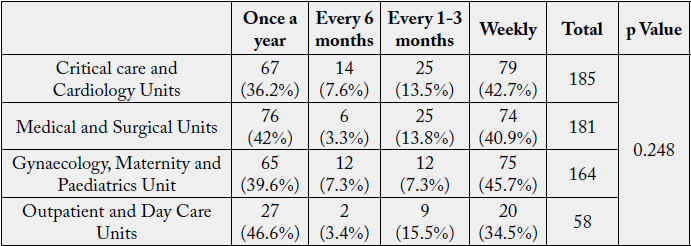
The exposure to chemicals toxic medication was found to be the highest among Critical care and Cardiology
Units, followed by Medical and Surgical Units, Gynaecology and Maternity and Paediatrics Units. Lowest
level of exposure was found in nurses working in Outpatient and Day Care Units where only 15.5%
respondents were exposed to the chemicals toxic medication on weekly basis, while 31.4% respondents in
Critical care and Cardiology Units, 29.8% respondents in Medical and Surgical Units and 30.5% respondents
in Gynaecology and Maternity and Paediatrics Units were exposed to the chemicals toxic medication on
weekly basis.
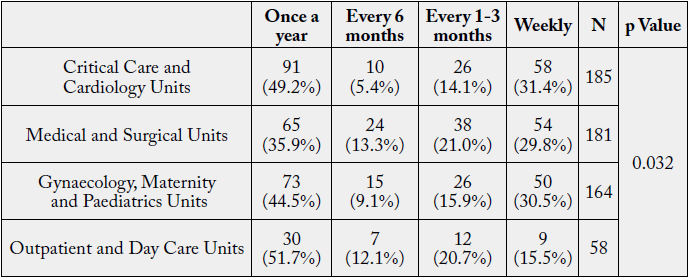
The p Value (0.032<0.05) derived from Chi-Square analysis of the data revealed a significant association among Unit and exposure of respondents to chemicals/ toxic medication.
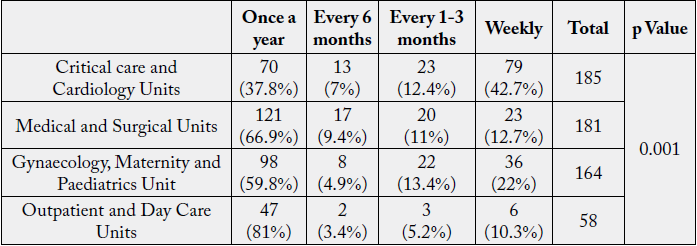
The exposure and irritation from disinfectants and sterilants was reported to be highest among respondents
working in Medical and Surgical units, followed by those in Critical Care and Cardiology Units; Gynaecology,
Maternity, and Paediatric Units compared to Outpatient Department and Day Care Units.
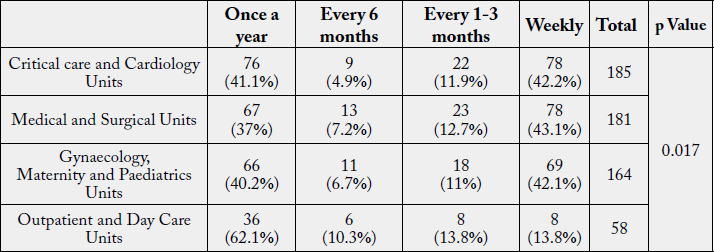
The p value (0.017<0.05) obtained from Chi-square test analysis revealed a significant association among Unit and irritation from disinfectants and sterilants.
Some highly toxic elements identified in surgical smoke are hydrocarbons, nitriles, fatty acids and phenols
[16].
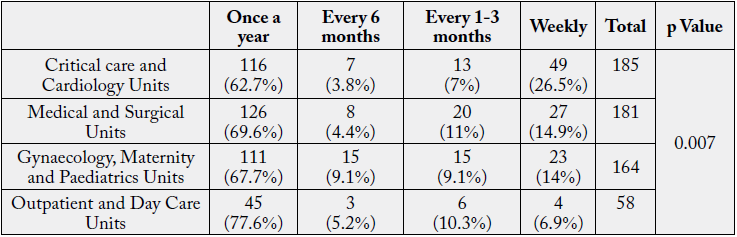
The p value (0.007<0.05) derived from Chi-square analysis revealed a statistically significant association among Unit and Exposure to toxic fumes.
In a similar study conducted by Moual et al., (2013) [17] to compare the risk of severe persistent asthma between the nurses of operation theatre(where there is a high risk of exposure to certain inhaled agents) with administrative nursing staff, the risk of persistent asthma was reported to be significantly higher in operation theatre nurses.
The effect of exposure to anaesthetic gases like chloroform, ether and nitrous oxide in higher concentration
leads to a headache, irritability, fatigue, nausea, drowsiness, confusion, and effect on liver and kidneys [18].
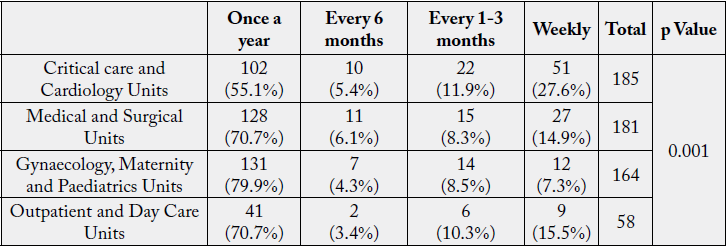
The p value (0.001<0.05) derived from Chi-square analysis revealed a statistically significant association among unit and exposure to anaesthetic agents. The exposure to anaesthetic gases was highest among respondents working in Critical care and Cardiology Units, Medical and Surgical Units, Gynaecology and Maternity and Paediatrics Units, compared to Outpatient and Day Care Units.
Falls are a growing concern in the health care industry. Yeoh et al (2013) [19] reported that non-fatal fallrelated
injuries are highest among the nursing profession, mainly in females aged between 45 to 64 years
and around 25% of falls result in 31 work days being lost. Also, risk of fall was observed more in nursing
aides when compared to registered nurses. Bureau of Labor Statistics (2009) [20]. reported that 11% of total
occupational injuries result from falls in the workplace.
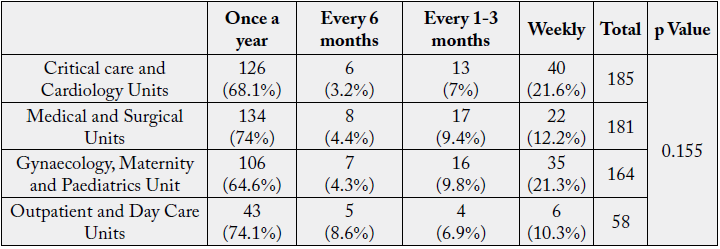
The p value (0.155>0.05) obtained from Chi-square analysis revealed a non-significant association among Unit and Risk of Slip and Fall.
The risk of fall or tripping mainly happens due to the wet floors or cluttered space. Within the outpatient department and day care unit the risk is least as there is adequate space within the work environment due to less equipments and cleaning of the floors are not as frequent as in in-patient units.
Health care professionals with type 1 hypersensitivity to natural rubber latex can continue to work by
reduction of exposure to latex and use of low-allergen non-powdered natural-rubber latex gloves whenever
possible [21].
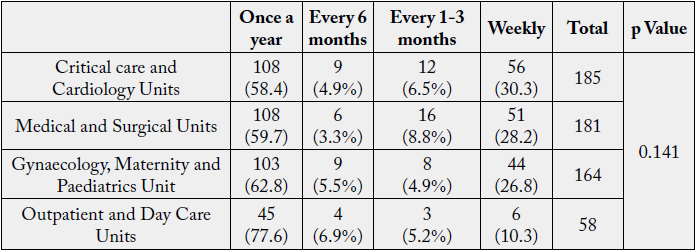
The p value (0.141>0.05) obtained from Chi-square analysis revealed a non-significant association among Area of Work (Unit) and Latex Allergy.
Radiation hazards are categorised as ionising radiation hazards (radionuclides in nuclear medicine, diagnostic
imaging and radiation therapy, X-Rays) and non- ionising radiation hazards (magnetic resonance imaging,
lasers, ultraviolet lights).
The p Value (0.001<0.05) obtained from chi-square analysis revealed a significant association among Unit and Exposure to Radiation.
A study by Chiou et al. (2013) [14] with same results found that nurses working in emergency rooms, intensive care units and wards have a more ill effect on health when compared to staff working in the outpatient department and administration. Nurses working in critical care units and operation theatres had high radiation exposures when compared to others.
As per the U.S Bureau of Labor Statistics (2017), hospital personnel’s routinely faced work-related injuries
due to lifting, moving or shifting of patients.
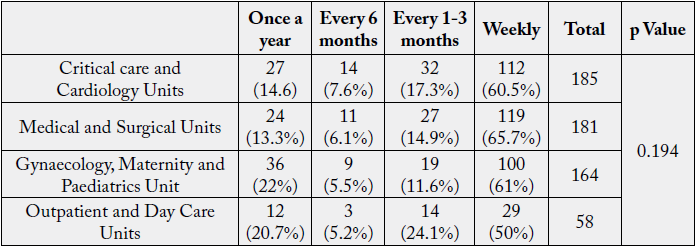
The p Value (0.194>0.05) obtained from chi-square analysis revealed no significant association between Unit and Low back pain.
Nurses working in intensive care units and neonatal intensive care unit nurses show the lowest prevalence of back pain and the highest prevalence of back pain is seen among medical intensive care unit staff. (Kyung & Sung, 2011).
Use of extreme force for lifting, pushing, pulling in awkward positions such as bending, twisting, repetitive
motion, vibration, working overhead can lead to ergonomic exposures.
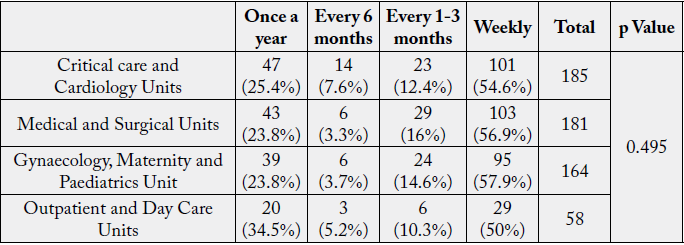
The p Value (0.495>0.05) obtained from Chi-square analysis revealed no significant association among Unit and experience of shoulder pain among nurses.
Lövgren et al. (2014) [22] reported that 50% respondents had constant prevalence and incidence of neck and shoulder pain even more than back pain which was reported by 40% respondents in a study conducted on student nurses.
Musculoskeletal symptoms are very common in nurses, especially the direct patient care providers [23].
The p Value (0.248>0.05) obtained from Chi-square analysis showed a non significant association among Unit and experience of wrist pain among nurses.
In a hospital setting, needle stick injury is a serious occupational hazard. The main factors which lead to
needle stick injuries are an urgency to complete work, shift duties, less experience, decreased skill etc [24].
The incidence of sharps injuries among health care providers was in nurses mainly due to recapping of the
needles [25].
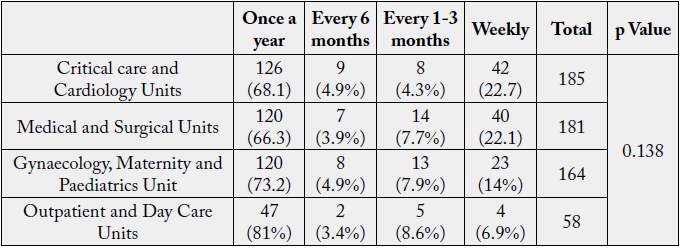
The p Value (0.138>0.05) derived from Chi-square analysis showed no significant association among Unit and incidence of needle stick injuries among nurses.
Factors that are associated with needle stick injuries are gender, age, department, and experience. Age and the area of work or the unit are the most important risk factor contributing to needle stick injuries [26].
Waleed et al. (2015) [25] reported that highest number of needle stick injuries occur in the emergency room followed by a dialysis unit.
The risk of infection is still a common risk to health care providers. Any hospital-acquired illness can lead
to economic consequences which can be assessed by the total number of sick leave or absenteeism caused
by the illnesses or by a cost of medical attention and compensation (Gestal, 2018). Health care workers
are at continuous risk of blood-borne viral infections with hepatitis B virus, hepatitis C Virus and human
immune-deficiency virus. During an epidemic like EBOLA and SARS or pandemic like COVID-19 health
care workers are at very high risk for infections due to their contact time with patients.
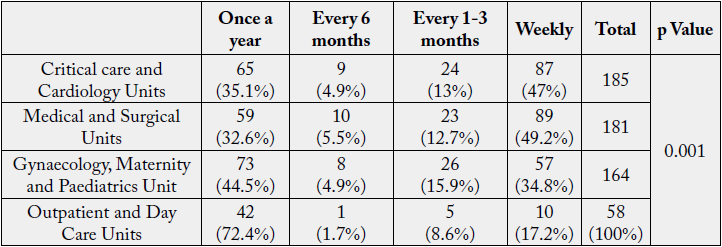
The p Value (0.001<0.05) determined by chi-square analysis revealed that there is a statistically significant association among Unit and exposure to blood borne pathogens and biological hazards.
Preventive measures include education, immunisation, adherence to universal precautions, post-exposure advice and prophylaxis [27].
Critical Care and Cardiology Unit were found to be the units with the highest risk of occupational hazards and injuries while the lowest risk was observed in the outpatient and day care unit. Chi square analysis of data revealed a significant association of clinical areas of work (Units) with exposure to blood borne pathogens & biological hazards, radiation, toxic fumes & anaesthetic agents, irritation from disinfectants & sterilants and chemical/toxic medication. On the other hand, a non-significant association was revealed among clinical areas of work (Units) with incidence of needle stick injuries; pain in wrists, shoulders & low back; latex allergy; and risk of slips and falls [28].
Conclusion
The healthcare workers face a lot of challenges in their day to day work life. There is a dire need to address
these occupational hazards so that they can be well taken care of in time, in order to reduce incidences of
illnesses and injuries among them. A strong medical workforce is the key to a healthy world. Proper precautions
and standard procedures should be an integral part of work for every individual, especially those working
in the healthcare work-sector. Injuries and hazards should be minimised in order to ensure a safe working
environment for the personnel. Wherever required, guidelines and interventions should be provided to
minimise the risk of workplace factors leading to injuries and illnesses.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!