Biography
Interests
Smith Nkhata, G.1* & Emmanuel Ayua2
1Department of Food Science and Technology, Natural Resources College, Lilongwe University of Agriculture and
Natural Resources, Lilongwe, Malawi
2Department of Food Science and Nutrition, University of Eldoret, Eldoret, Kenya
*Correspondence to: Dr. Smith Nkhata, G., Department of Food Science and Technology, Natural Resources College, Lilongwe University of Agriculture and Natural Resources, Lilongwe, Malawi. Email: snkhata@luanar.ac.mw
Copyright © 2019 Dr. Smith Nkhata, G., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Lycopene and β-carotene are common dietary carotenoids found in fruits and vegetables. These carotenoids have health benefits primarily due to their anti-oxidant properties. However, in cancer chemoprevention, these antioxidant carotenoids slow down cancer initiation and progression through various mechanisms independent of antioxidant effect. Most importantly, they induce cell cycle arrest and apoptosis consequently, slowing down proliferation of cancerous cells. The carotenoids up-regulate PPAR-γ which is a ligand-activated transcription factor known to regulate numerous cellular activities such as cell survival, growth, differentiation and apoptosis. These cellular activities regulate morphological aspect of cells and are very vital in cancer cells and tumor development. Unfortunately, accumulating data on these effects are derived from studies that used pharmacological doses putting in doubt any beneficial effect on cancer chemoprevention from dietary sources. However very few studies have demonstrated these effects from dietary sources (physiological dose).This review focuses on four major mechanisms of lycopene and β-carotene in chemoprevention and highlights some of the challenges and gaps that need to be addressed in using these bioactive compounds from dietary sources for cancer management and prevention.
Introduction
Nutrition and health organizations recommend high intake of fruits and vegetable because they are associated
with decreased incidences of chronic diseases such as type 2 diabetes, cardiovascular diseases and cancer
[1]. Dietary guideline for Americans recommends 2.5 and 2.0 cup-equivalents of vegetables and fruits
per day [2]. Several studies have attributed beneficial health effects of fruits and vegetables to carotenoids
[3,4,5]. Carotenoids are fat-soluble antioxidant derived from the isoprenoid biosynthetic pathway. The most
common carotenoids in diet are lutein, zeaxanthin, α-carotene, β-carotene, lycopene and β-cryptoxanthin.
Carotenoids such as β-carotene, α-carotene and β-cryptoxanthin possess provitamin A (PVA) activity
because they can be metabolized in the gut and liver to vitamin A while zeaxanthin and lutein are the
major carotenoids in the macular region of human retina where they protect the eye against age-related
macular degeneration (AMG). Most of these protective effects of carotenoids are due to their antioxidant
capacity as they can quench free radicals such as peroxyl radicals but also scavenge singlet oxygen [6,7]
thereby reducing oxidative stress due to reduced accumulation of reactive oxygen species (ROS). Oxidative
stress has been implicated in many pathophysiological conditions such as cardiovascular diseases, cancer and
obesity [1,8,9]. Evidence also suggests that carotenoids reduce oxidative stress by interacting with nuclear
factor erythroid 2-related factor 2 (Nrf2) pathway and enhance its translocation to the nucleus where it
activates phase II (detoxifying) enzymes and antioxidant enzymes such as superoxide dismutase (SOD) and
glutathione peroxidase (GPx) [1]. Moreover, carotenoids have anti-inflammatory properties. It has been
reported that carotenoids block translocation of nuclear factor kappa B (NF-kB) to the nucleus and inhibit
the downstream production of pro-inflammatory cytokines such as interlukin-8 (IL-8) and prostaglandin
E2 (PGE2) [1].
Protective effect of high carotenoid rich foods against oxidative stress and inflammation are supported by nutrition intervention studies and animal models. Consumption of 330mL/day tomato juice (40mg lycopene), 330mL/day carrot juice (22.3mg β-carotene and 15.7mg α-carotene) and 10g/day of dried spinach (11.3mg lutein) in milk/water resulted in reduction in DNA oxidation as evidenced by reduced strand breaks in peripheral lymphocytes from health individuals [10]. Biomakers of oxidative stress (8-iso- PGF2α) and inflammation (thromboxane B2, prostaglandin E2 metabolites, and hsC-reactive protein) were reduced after 3 week carrot juice intervention in overweight breast cancer survivors after consuming 8 ounces of β-carotene rich fresh BetaSweet or Balero orange carrot juice [11].
Lycopene and β-carotene are commonest dietary carotenoids and are major carotenoids detected in human plasma. They are primarily obtained from consumption of fruits, vegetables and more recently high carotenoid biofortified maize (only β-carotene) and can therefore be easily incorporated in a diet without changing dietary pattern. The main sources of lycopene are tomatoes and water melon while sources of β-carotene include green leafy vegetables, pumpkins, potatoes, biofortified maize and biofortified cassava. Many studies, clinical intervention, animal and cell models have shown their anticancer properties in a time and dose dependent manner [12,13]. While there is a general consensus that these carotenoids slow down cancer progression by reducing cell viability and cell cycle progression, the mechanism underlying these actions are not clear and predictable. The exact molecular mechanism of carotenoids differs from cancer to cancer and stage to stage. Variations are also evident within the same type but different cell lines depending on estrogen receptor (ER) or progesterone receptor (PR) or human epidermal growth factor receptor 2 (HER2) status [13]. For example, both lycopene and β-carotene induced cell cycle arrest and apoptosis [14,15] and inhibited cancer cell proliferation [13,16] in various human cancer cell lines. However, β-carotene did not have any effect on cell proliferation and differentiation process of leukemic cell lines [17]. Unexpectedly, lycopene increased proliferation of LNCaP cells and had weaker effect on prostate cancer cells (PC-3 cells) and these effects were dependent on androgen sensitivity [18]. These results make it very difficult to predict the chemopreventive effect of both lycopene and β-carotene across different cancers. However, a vast body of evidence points to the protective effect of these compounds in cancer management.
Evidence from Epidemiological Studies
There is strong evidence of the inverse association between fruits and vegetable consumption and breast [19]
and prostate [20] cancer risk. Prospective analysis has shown lower prostate [21] and breast [22] cancer risk
in men and women, respectively, with elevated plasma lycopene level. However, reports are conflicting as the
effects of fruits and vegetables on various cancers are dependent on the biomakers being assessed and ER
status. In a pooled analysis and prospective cohort study, no association was observed between fruits and
vegetable intake with general breast cancer though fruits and vegetable intake was inversely associated with
risk of estrogen receptor-negative (ER-) but not estrogene receptor-positive (ER+) tumors [19]. Though
these effects are not specific to β-carotene and lycopene, as fruits and vegetables contain other bioactive
compounds in addition to these carotenoids, studies have tried to elucidate contribution of carotenoids
toward such benefits [23]. Specifically, human clinical trials have demonstrated that the breast cancer risk is
inversely associated with various carotenoids including β-carotene [23,24]. Both β-carotene and lycopene
were inversely associated with ER- breast cancer in meta-analysis of 18 prospective cohort studies with
non-significant progesterone receptor-negative (PR-) and PR+ association [24]. These studies have shown
that carotenoids or fruit and vegetable consumption may be protective against ER- but not ER+ indicating
that other mechanisms independent of steroid hormones mediate ER+ tumors. It is therefore reasonable
to believe that protective mechanism of carotenoids such as antioxidant effect observed in ER- tumors
might not overcome tumorigenic effect from protumorigenic stimuli perpetuated my steroid hormones in
ER+ tumors (steroid hormones may override preventive effect of carotenoids in ER+ tumors). Another
explanation could be that ER+ may possibly need a higher dose of these carotenoids than those obtained
through fruits and vegetable consumption to elicit a protective effect. This was confirmed by Gloria et al
study in which lycopene reduced cell viability only at higher concentration in ER+ cells only while it did
not have effect on ER- cell after 48 hours [12]. In contrast, high dose β-carotene, unlikely to be achieved at
physiological level, either promoted proliferation or had weaker effect on androgen sensitive LNCaP cells
[18]. Taken together these data suggest that androgen receptor (AR) status determine the effect of lycopene
and β-carotene on tumor growth and progression. Therefore, it is most likely that lycopene and β-carotene
may reduce cell viability of AR sensitive tumors depending on concentration and time of exposure and that
lower concentration seem to have insignificant effect on ER+ while the same concentration might have
effect on ER- tumors.
AR Status is Related to Risk of Breast and Prostate Cancer
Cancer initiation is a multifactorial phenomenon. Cancer develops because of different factors that are
either extrinsic or intrinsic or a combination of both. Cancers are caused by mutations that are inherited,
environmentally induced and/or errors during DNA replication [25]. Most extrinsic factors involve dietary
patterns, life style and environmental exposure to carcinogens that can be positively modified thereby
reducing the risk of developing cancer. Unfortunately, intrinsic factors are more difficult to modify as they
may involve genetic alterations or reproductive and hormonal factors. For example, 15% of all cancer deaths
in the United Kingdom are believed to be attributable to reproductive factors such as those occurring during
puberty, pregnancy, breastfeeding and post-menopause [26]. AR affects the invasiveness of breast tumors
[27]. Most importantly there is strong evidence that high circulating level of estrogen increases risk of breast
cancer in post-menopausal women and this is supported by the fact that users of exogenous hormones have
a 25–35% higher risk of developing breast cancer than those that have never used them [27]. In addition to
the physiological risk factors, dietary factors such as high fat diet increases prostate tumor growth [28] while
diet rich in phytochemicals such as soy isoflavone [29] and alpha-tocopherol [30] has been associated with
protective effects in prostate cancer patients.
Similarly, prostate cancer initiation and progression is also dependent on AR. While AR is important for normal growth and development of the prostate gland, studies show strong relationship between cellular AR level in both primary and metastatic lesions [31]. Among different mechanisms, AR is transactivated by interlukin-6 (IL-6) produced by many cells including prostate and immune cells which may lead to downstream signaling that can activate different signaling pathways including mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3 kinase (PI3K) pathways [32]. Elevated circulating IL-6 levels have been associated with advanced stage, distant metastases, metastasis-related morbidity and decreased survival of prostate cancer patient [32]. Production of IL-6 is high in obese individuals. Luckily the risk of prostate cancer can be modified by dietary means. There is reduced prostate cancer risk among men with elevated plasma level of lycopene [20,21] indicating that lycopene can reduce or delay initiation or progression of prostate cancer. This association has been confirmed in cell culture model of prostate and breast cancer in a dose and time dependent manner. Both lycopene and β-carotene induced cell arrest and inhibited proliferation in AR sensitive MCF-7 breast cancer cells [12] and LNCP cancer cells [33] by different mechanisms.
Mechanism of Action of Lycopene and β-Carotene in Breast and Prostate Cancer
Chemoprevention
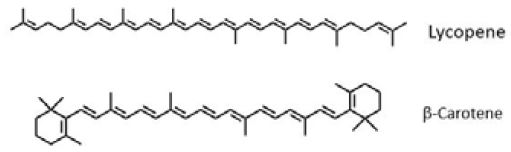
Lycopene and β-carotene are associated with decreased incidences of cancer by similar mechanisms.
Structurally, they are all polyunsaturated with β-carotene having cyclic β-ionone rings at either end while
lycopene does not have the rings (acyclic) (Figure 1). The major mechanism by which lycopene and β-carotene
negatively affect cancer cells is through modulation of cell cycle progression and proliferation. Cancer cells
are unable to progress through the first gap (G1) phase and this effect is dependent on type of cancer cells,
dose and time of exposure [12]. Moreover, both lycopene and β-carotene are potent antioxidant known to
scavenge free radicals thereby reducing accumulation of reactive oxygen species (ROS) which may destroy
DNA and initiate mutation [14,34,35]. By breaking production of ROS lycopene and β-carotene protect oxidation of proteins and membrane lipids. Oxidized protein and membrane lipids disturb the integrity
of DNA and cell membranes and may initiate mutation and inflammation, respectively [10]. Inconsistent
with this notion, β-carotene induced ROS generation and cytochrome C enzymes which was attenuated
by glutathione (GSH) in MCF-7 [36] indicating that β-carotene can be a pro-oxidant depending on dose
and redox potential of the environment. However, the increased ROS generation paralleled upregulation of
p21 gene which is a potent inhibitor of cyclin dependent kinase. In this regard β-carotene induced ROS
dependent apoptosis in MCF-7 mammary cell lines [36]. Therefore, β-carotene effects on cancer initiation
and progression is not limited to antioxidant properties only but rather to its pro-oxidant effect too.
Increase in oxidative and nitrosative stress has been reported in prostate cancer [37,38] with subsequent decrease in natural antioxidants such enzymes as glutathione peroxidase (GxP) and superoxide dismutase (SOD). Moreover, breast cancer cells are more susceptible to oxidation than normal cells [39]. Consistent with depletion of natural antioxidant hypothesis, SOD3 overexpression was associated with inhibition of cell proliferation, migration, and invasion in PC-3 cell lines [40]. Therefore, low SOD3 expression in prostate cancer patient might increase prostate cancer invasiveness. Since natural anti-oxidant defense mechanism is reduced in obese individual [41], this might partly explain why obese individuals have higher risk of developing cancer than their lean counterparts. Consequently, both β-carotene and lycopene, being potent antioxidants, can increase the antioxidant capacity of the body which can help reduce free radicals that may damage DNA. This review focuses on four main mechanisms of lycopene and β-carotene in breast and prostate cancer chemoprevention. These mechanisms include induction of cell cycle arrest and apoptosis, upregulation of peroxisome-proliferator activated receptor gamma (PPAR-γ), up-regulation of ROS generation, alteration of mevalonate pathway and interference with insulin-like growth factor 1(IGF-I) signaling.
Induction of cell cycle arrest and apoptosis perse do not provide detailed mechanistic information on how
β-carotene or/and lycopene affect cell growth and proliferation. However, it gives a platform for further
examination of mechanistic events occurring preceding cell cycle arrest and apoptosis. Both lycopene and
β-carotene are known to induce cell cycle arrest and apoptosis in different cancer cell types. Lycopene
decreased survival fraction and induced cell cycle arrest in G0/G1 phase of three different human breast cancer cell lines at physiologically achievable concentration [13]. These effects were dependent on cell line
and time of exposure with prolonged exposure producing profound effects. The inhibitory effect was higher
in triple-negative MDA-MN-468 cells while least in ER/PR positive MCF-7 and ER/PR negative and
HER2 positive SK-BR-3 cells indicating that inhibitory effect of lycopene depends on AR status. The
inhibitory effect paralleled decreased cyclin D1 and increase in bax protein expression in a cell specific
manner. Lycopene also inhibited phosphorylation of Akt and downstream mTOR in triple negative cells.
The Akt/mTOR signaling pathway is important for controlling cell survival and apoptosis. Interestingly,
lycopene did not affect anti-apoptotic proteins such as Bcl-xL in all cell lines [13].
Consistent with ER status hypothesis lycopene administration increased expression of (breast cancer 1) BRCA1 and BRCA2 genes in ER+ (MCF-7 and HBL-100) while it decreased gene expression in ER- (MDA-MB-231) cell lines [42]. BRCA1 and BRCA2 are tumor suppressor gene and their expression is regulated with cell cycle and associated with proliferation in normal and tumor-derived breast epithelial cells [42]. In a separate study when three different human breast adinocarcinoma cells lines (MCF-7, MDAMB- 235, MDA-MB-231) were exposed to different concentration of lycopene and β-carotene there was different but dose and time dependent effect on cell viability [12]. Lycopene reduced cell viability of estrogen receptor positive (ER+) MCF-7 only at higher concentration while it did not have any effect on estrogen receptor negative (ER-) MDA-MB-231 after 48 hours. Lycopene was most effective at all doses after 48 hours in reducing viability of MDA-MB-235 regardless of concentration. Interestingly, cell viability for all cell lines were reduced after 98 hours independent of concentration highlighting importance of lengthy exposure to carotenoids on cell viability [12]. Consistent with Takeshima et al., lycopene did not have effect on MDA-MB-231 after 48 hours but it had greatest reduction after 98 hours highlighting the importance of prolonged exposure [13]. Unlike lycopene, β-carotene significantly reduced MCF-7 cell viability after 48 hours to a higher extent than after 98 hours while other cell lines were reduced to the same extent. The difference in time taken to produce effect between β-carotene and lycopene in these studies may be due to preferential uptake of β-carotene by hepatic stellate cells [43,44] leaving lycopene in circulation longer.
Inhibition of cell proliferation and induction of apoptosis were probable reasons for reduced cell viability. Lycopene and β-carotene induced cell cycle arrest mainly in the G0/G1 or G2/M phases depending on cell type and carotenoid concentration. Inhibition of cell cycle progression in the G1 and S phase has also been reported for MCF-7 mammalian cells [45]. The number of apoptotic cell increased in dose, time and cell type dependent manner. The ability of β-carotene to induce apoptosis has been confirmed in gastric cancer AGS cells where activation of caspase-3 protein, a molecular marker for apoptosis, was increased after treatment with β-carotene [34]. It is suggested that apoptosis induced by β-carotene is associated with ROS generation in colon adenocarcinoma and HL-60 human leukaemia cell types [46]. Treatment of human leukemic T cell line Molt 4 with β-carotene triggered caspase 2 activation and feedback amplification [47] indicating increased cell apoptosis. Similarly, the inhibitory effect of lycopene on cell cycle progression was mediated through down-regulation of cyclin D possibly due to retention of p27 in the cyclin E- cdk2 complex resulting in inhibition of cdk2 kinase activity which resulted in inhibition of G1/S transition [48]. These data point to the fact that lycopene induce cell cycle arrest at G0/G1 phase and down regulated cyclin D1 and up-regulated p21 and p27 regardless of ER and HER2 status.
β-carotene is a well know antioxidant and/or pro-oxidant depending on the concentration and redox
potential of the environment in which it acts. In low concentration it provides antioxidant activity while at
high concentration especially in the presence of oxidative stress, it behaves as pro-oxidant propagating free
radical induced reactions, consuming endogenous antioxidants and inducing DNA oxidative damage [46].
It is well known radical scavenger in in-vitro models [49]. However, prooxidant activities have been reported
both in-vitro and in-vivo [50].
PPAR-γ pathway has been reported to play a role in breast cancer cell differentiation [51]. At that time the mechanism behind β-carotene inverse relationship with breast cancer was not clear. PPAR-γ was a candidate for β-carotene mechanistic study because it is implicated in many processes related to cellular development and differentiation. Few studies found that the chemopreventive effect of β-carotene results from its ability to up-regulate PPAR-γ expression and ROS production in MCF-7 cancer cells (36; 46). PPAR-γ is a ligand-activated transcription factor known to regulate cellular development such as cell survival, growth, differentiation, and apoptosis [51,52]. p21 is cyclin-dependent kinase inhibitor which inhibits cell cycle progression leading to G1 arrest and was activated by PPAR-γ in ROS dependent manner [36]. The ability of β-carotene to increase ROS generation in WiDr colon adenocarcinoma and Hl-60 human leukemia [46] and Molt 4 [47] cancer cells have also been reported. Cyclin-dependent kinases are responsible for cell cycle progression and cell proliferation. Up-regulation of p21 was attributed to pro-oxidant properties of β-carotene which is consistent with results from other studies [14]. Therefore, anti-proliferative effect of β-carotene is attributed to its ability to activate PPAR-γ which activated p21 in a ROS dependent mechanism. Moreover, in the same study the inhibition of COX-2, an enzyme responsible for inflammation and pain, was mediated through PPAR-γ pathway since PPAR-γ antagonist was able to attenuate PPAR-γ effect [36].
The beneficial effect of β-carotene in up-regulating PPAR-γ looks counterintuitive as PPAR-γ is activator of adipogenesis and fatty acid storage [53] and increased expression is associated with obesity which is associated with increased cancer risk [54,55]. However, in addition to up-regulating p21, PPAR-γ effects is associated with its anti-inflammatory properties due to its ability to reduce expression of resistin and tumor necrosis factor alpha (TNF-α), which induce insulin resistance and are both proinflammatory [53,56]. Moreover, PPAR-γ activation by its ligand induces terminal differentiation of malignant breast epithelial cells and causes dramatic morphological and molecular changes that are characteristic of a more differentiated but less malignant state in breast cancer cells [57]. This is supported by the notion that forcing cell to complete terminal differentiation can be used to treat human malignancies as ‘tumors fail to express appropriate level of molecular and morphological markers of the terminally differentiated state’ [57].
Evidence that lycopene induce G0/G1 or G1/S cell cycle arrest is overwhelming and epidemiological
studies support the protective effect of lycopene against some cancers. Both intake of tomatoes and plasma
lycopene levels are reported to have inverse relationship with prostate cancer [58]. Studies have supported effectiveness of lycopene at reducing tumor size [59] inhibiting the growth of non-neoplastic human prostate
epithelial cells [60] and induction of mitochondrial apoptosis in LNCaP cells [61]. There are a number of
mechanism by which lycopene produce these effects. Lycopene is a potent antioxidant as it reduced ROS
production in a dose dependent manner [33] and therefore it could be effective at reducing oxidative stress
that may cause DNA damage. However, antioxidant mechanism does not explain all the beneficial effect
of lycopene. Other mechanisms include modulation of cyclo-oxygenase pathways [33] and modulation of
IGF-I signaling pathway [45]. Additionally, lycopene induced cell growth inhibition by altering mevalonate
pathway and Ras signaling in LNCaP cancer cell lines in a dose dependent manner [33]. This effect preceded
lycopene inhibition of cholesterol synthesis [33].
Lycopene inhibited expression of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase and thereby modulating the mevalonate pathway. Mevalonate pathway is important for the synthesis of intermediates such as geranyl pyrophosphate and farnesyl pyrophosphate which may regulate transcriptional and post transcriptional events but also bind to Ras protein on cysteine residue [33]. This binding is necessary as it enables Ras protein to attach to plasma cell membrane. Moreover, farnesylation is involved in malignacy and Ras protein require farnesylation [33] and low molecular weight guinosine triphosphatases (GTPases) require prenylation to promote tumorigenesis [62]. Farnesylation is required for Ras cell membrane localization. The major factor in Ras activity is its translocation from the cytosol to the plasma cell membrane [33]. Thus inhibiting HMG-CoA reductase prevented membrane localization of Ras due to lack of farnesylation and affected Ras activity. Consistent with this, the GTPase which depend on farnesylation for their activities remained inactive and incapable of activating the MAPK cascade, which ultimately suppressed the Ras-dependent activation of NF- κB. These events were followed by increased number of apoptotic cells. However, when lycopene was used in the presence of mevalonate the growth inhibitory effect of lycopene was removed indicating that mevalonate pathway has an effect on anticancer activity of lycopene. The inhibitory effect was higher in cell lines possessing Ras mutation than those that do not have suggesting Ras signaling could be a target for lycopene chemotherapy [33].
It is known that IGFs are important in tumor formation and cell proliferation and a strong positive
associations between IGF-I and prostate cancer and breast cancer have been reported [63,64]. Therefore,
use of lycopene and β-carotene as chemopreventive strategy in cancer prevention holds promise. Effect of
lycopene on cancer cell growth is conflicting as some studies have shown it causes cell death due to toxicity
[12,33] while other studies, though agreeing to its anticancer properties, indicated that lycopene do not
induce cancer cell death but rather interferes with IGF-I signaling [45] and therefore slows IGF induced
cell growth. Taken together, it suggests that apart from inducing necrotic and apoptotic effect [12] the
inhibitory effect of lycopene might also depend on its ability to interfere with mitogenic insulin-growth
factor 1(IGF-I) receptor signaling and cell cycle progression [45,65].
Epidemiological studies have shown that high plasma IGFs are major risk factors for both prostate and breast cancers [63,64]. Lycopene seem to reduce the IGF-I stimulation of tyrosine phosphorylation of insulin receptor substrate 1(IRS-1) and binding capacity of activating protein-1 (AP-1) transcription complex with subsequent increase in membrane-associated IGF-binding proteins (IGFBP) [45]. IGF-I binds to IGF-I receptors which leads to activation of downstream signaling [66] that include genes regulating tumor formation and progression [67] and this property of IGF makes it as a target for chemoprevention. In addition, lycopene was able to suppress IGF-1-stimulated growth and strongly inhibited proliferation of MCF-7 mammary cells and its inhibitory concentration was 10 folds lower than β-carotene indicating that lycopene is a more potent inhibitor of mammary human cancer cell proliferation than β-Carotene [68]. Moreover, MCF-7 cells became resistant to all-trans retinoic acid, a metabolite of β-carotene, after a long term exposure to this metabolite indicating growth inhibitory effect of retinoic acid could be lost during prolonged exposure as cell may acquire resistance [65]. Nevertheless, the anticancer effect of both lycopene and β-carotene partly depended on effects on IGF-I signaling. The inhibitory effect of lycopene on IGF signaling was associated with suppression of IGF-dependent cell cycle progression of serum starved cells [45] indication inhibitory effect is not dependent on lycopene toxicity but on interference with IGF-I receptor signaling. Interestingly, this effect was achieved at physiological level normally found in blood of people consuming medium to high levels of tomato products.
Challenges to Using Dietary Sources for Lycopene and β-Carotene for Chemoprevention
Despite the promising discoveries in use of carotenoids as chemopreventive agents there are still some
challenges that need to be addressed regarding the bioactivity of these compounds and dietary patterns
of the population. While many studies demonstrate anticancer properties of lycopene and β-carotene, few
studies have achieved those effects at physiological concentrations. Achieving that level requires medium to
high consumption of carotenoid containing fruits and vegetables. Getting and maintaining the population
on such diet still remains a challenge as fruits and vegetable consumption in many countries including
USA is below recommended intake across all age groups (2, https://ourworldindata.org/diet-compositions).
Moreover, the obesogenic (high fat) diet in many developed countries may overshadow any such benefits.
With the possibility that high level β-carotene may induce ROS production and increase progression of some
cancer, it is very unlikely that ROS dependent apoptosis showed in some studies [33] would be relevant to
humans. This makes extending these potential benefits to humans difficult as ROS may damage DNA and
induce pro-inflammatory cascade that may create an environment conducive to cancer progression.
Most of the bioactive compounds including lycopene and β-carotene have low bioavailability. Increasing fat content in the diet improves their bioavailability. However, fats are implicated in many metabolic disorders such as diabetes and obesity and increasing their bioavailability by high consumption of fats may not be accepted by people trying to reduce dietary fat intake in developed countries. However, this may be an opportunity that must be exploited in developing countries where dietary fat still remains low. On the contrary, countries already on high fat dietary intake, the bioavailability of carotenoids would be relatively higher than in a similar population that do not consume a similar amount of fats. Therefore, more studies would be needed to determine whether a generally high fat diet would work to this potential advantage and whether the high fat would not obscure any potential chemopreventive gains resulting from consumption of lycopene and β-carotene. Moreover, the finding that cancer cell can develop resistance to β-carotene [65] is sickening. This may possibly be overcome through synergistic effects of different phytochemicals that have different growth inhibitory mechanisms. There are many studies that support combination of different phytochemicals to make use of the synergistic effect of these compounds. This may help to overcome cancer cell resistance to a particular compound. In this regard, it would be hard to attribute any observed benefit to lycopene or β-carotene since dietary sources provide many different bioactive compounds.
The biggest gap that still exists is mimicking the complex human physiology in developing or designing cancer cell models. Many cells specific to studying particular cancer have been developed. While they try to mimic cancer cells, they do not mimic cancer microenvironment typical of cancer cell in human body. Cancer cells in tumors can modify the tumor microenvironment that favors their growth and proliferation. It is this ability to modify their environment that make cancer cell proliferate and metastasize, a component that is not reproduced in many cell culture models. Therefore, chemoprevention strategy primarily designed based on results from isolated cancer cells do not perform as expected when used as chemopreventive agents in humans. Xenograph techniques have been used to address this shortfall but they do not mimic complex tumor microenvironment well.
Conclusion
Since β-carotene and lycopene can interfere with many pathways that affect tumorigenesis and carcinogenesis,
and that their use do not pose any severe side effects, are found in regular human diet, they have potential
to be used as chemoprevention agents. Though some studies have demonstrated these effects within ranges
that could be achieved through normal dietary intake, unfortunately, many studies achieve these effects
at pharmacological concentration that cannot be replicated under physiological conditions. The challenge
is getting and maintaining people on high fruits and vegetable diets that may help achieve the lycopene
and β-carotene plasma levels associated with chemopreventive effects. Promotion of high consumption
of lycopene and β-carotene rich foods is practical but getting the plasma level that can elicit cancer
chemoprevention still remains a challenge.
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethical Review
This study does not involve any human or animal testing.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!